The shoulder consists of a ball (humeral head) and a socket (glenoid). The muscles around the shoulder act to elevate the arm. The large outside muscle is the deltoid and deep to that is the rotator cuff – this is a combined tendon and inserts into a prominence on the humeral head known as the greater tuberosity. Four muscles contribute to the rotator cuff tendon: the supraspinatus, infraspinatus, teres minor and the subscapularis. The supraspinatus tendon is the one most commonly affected.

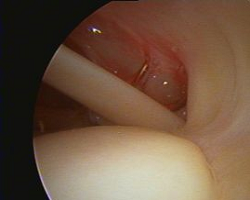
(Left )Anatomy of the rotator cuff: As seen here, four muscles contribute to the rotator cuff.(Right)Arthroscopic view of the rotator cuff from inside the joint.
ROTATOR CUFF TEARS
Most tears are as a result of degeneration or “wear and tear”. The circulation to the tendon becomes impaired in older people and leads to degenerative tears. Another cause may be impingement by the overlying acromial bone spur. (see the section on “Impingement”) Injuries (falls, etc.) can result in “traumatic” tears when a fall or an other forceful mechanism tears the tendon off its insertion site on the greater tuberosity.

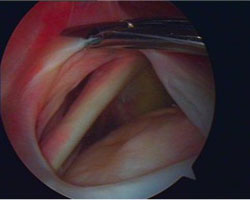
Rotator cuff tear: Diagrammatic view (left) and arthroscopic view (Right).
DIAGNOSIS
1. Clinical: Symptoms of a Rotator Cuff Tear
Pain is usually experienced in the shoulder and down the outer aspect of the upper arm, often worse at night. There may be an increase in the pain and a weakness experienced when elevating the arm. Occasionally, a “hooking” feeling is experienced, especially bringing the arm down to waist level from an overhead position.
Impingement of the cuff muscle under the shoulder bone (acromion) can result in a tear.
2. Radiological:
Xrays show changes in advanced stages only, when arthritis has set in.
Ultrasound is an excellent modality for accurate diagnosis of rotator cuff tears in early stages. This can be performed in the office and is inexpensive.
MRI shows cuff tears and also show the condition of muscle; muscle wasting (atrophy and fatty tissue) are associated with retearing and progression to arthritis.
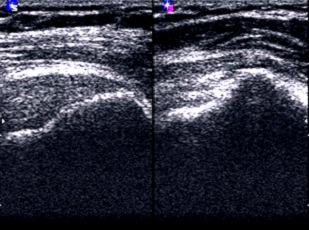
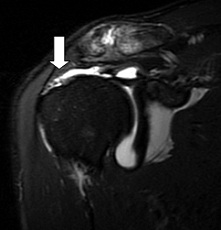
Radiological diagnosis of a rotator cuff tear: Ultrasound (Left) an MRI (right) showing a cuff tear.
SURGICAL REPAIR OF THE ROTATOR CUFF
The question is if a rotator cuff tear should be repaired or left for “conservative” treatment – that would imply cortisone injections, physiotherapy, etc. It is a fact that a rotator cuff tear can become pain free in certain individuals but normal power is unlikely to return.
The question, however, revolves around predictability: in certain individuals the tears may become painless and symptom free. A large proportion of the tears, however, may gradually increase in size and the muscle may deteriorate to the extent that it becomes irreparable. Unfortunately we have no way of predicting which tears will result in a poor outcome. On the other hand, we know that following repair, the outcome is predictably good.
THE OPERATION
We usually do this by means of an arthroscope (“key hole surgery”). Four tiny holes (3mm) are made around the shoulder for passage of the instruments. The bone is “roughened” to enable the tendon to heal to it. Bone anchors (tiny devices with sutures or “thread” attached) are drilled into the bone and the tendon is repaired to the bone with these sutures.
Healing of the tendon to the bone takes around 6 weeks and even longer to strengthen – up to 6 months. Ingrowth is a long tedious event.
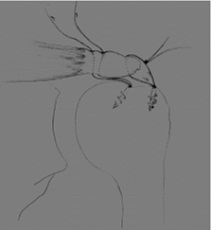



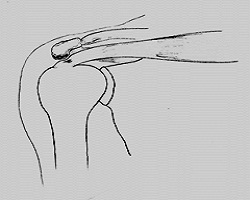
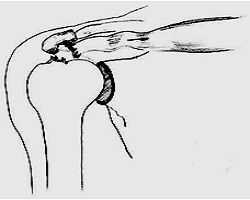
Rotator cuff repair: Diagrammatic view (top) and Arthroscopic view (bottom)
AFTER THE OPERATION
Your stay in hospital will be short – usually one day. A sling will be worn for about 6 weeks to protect the repair. During this time you will not be allowed to do active movements of the arm. The physiotherapist will instruct you how to do passive motion exercises – to lift the arm with the other arm, keep the arm mobile without using the newly repaired muscle by demonstrating passive motion exercises.
PAIN / DISCOMFORT FOLLOWING THE OPERATION
After arthroscopic repair of your torn rotator cuff, there will be some pain, varying from a few days to weeks, after which the shoulder should return to normal. A small percentage of patients may develop a “frozen shoulder” – the shoulder is stiff and painful for a few weeks, but this is temporary and always resolves. The cause is unknown but it is almost as if nature is trying to “protect” the repair.
RECOVERY TO NORMAL ACTIVITIES
Taking into account that the majority of rotator cuffs tear as a result of degeneration (“wear and tear”) and poor vascularity and not necessarily as a result of trauma, it implies that the tendon not only has to heal back to bone, but the abnormal tendon tissue has to be replaced by new tissue in addition. Levels of normal, everyday activity, can be reached within weeks, but more demanding activities may take up to 4-6 months (overhead sports, etc.).
It needs to be re-emphasised that the post-operative period may be long and frustrating. The final outcome, however, is good or excellent: in our unit we have performed over 600 cases in this manner and the result in more than 90% is excellent. Remember that the alternative is to leave the torn tendon “as is”. These tendons never heal and may become irreparable at a later stage, which could lead to chronic pain and disability. There is no doubt that repairing a torn tendon is the best option for your shoulder.
POST-OPERATIVE REHABILITATION
Passive motion should be done regularly but active motion avoided for 4-6 weeks. Passive motion means that the arm is moved by another force. E.g. the arm can be lifted by the other arm or holding on to a pulley.
Active motion: The muscles of the shoulder are used to move the arm. As these are newly repaired, the repair can be re-torn. Therefore active motion becomes safe only after 6 weeks.
THE SLING
On waking from the anaesthetic your arm will have been placed in an immobilisation type of sling. In some cases a sling with a built-in pillow might be used to keep the arm away from the body.
The main purpose of the sling is to remind you not to actively elevate the arm.
Make sure that the sling fits comfortably – inform us if it needs to be changed. Occasionally a larger sling needs to be fitted. (eg. compression of nerves at the wrist causing tingling and swelling of the hand)
EVERYDAY ACTIVITIES (HOW TO MANAGE)
Your physiotherapist and of course, ourselves, will assist you with this type of information.
There are, however, activities that will be problematic or even impossible in the few weeks following the operation and one should take these into consideration when planning your operation.
REMEMBER THAT YOU SHOULD NOT ELEVATE THE ARM AND THIS WOULD FOR EXAMPLE BE THE CASE IN DOING THE FOLLOWING
- Doing hair, brushing teeth, shaving and getting dressed particularly when the dominant arm was operated.
- Other activities could also be difficult, such as tying shoe laces, knotting a tie and doing up / undoing a bra.
- Driving a car is possible, but please discuss the timing of this. (power steering, etc)
- Sleeping: you should not sleep on the affected shoulder for a few weeks, and it may be painful to lie on anyway. There is often night pain for a few weeks following surgery. Painkillers and sleeping tablets may be required.
RETURN TO WORK
The question of when it will be safe / comfortable to return to work depends on the duties one is required to perform. As long as the arm is not used actively, it is safe. For example, working on a computer with the elbow resting on the table, is acceptable.
PROGNOSIS (SUCCESS RATE)
More than 9 out of every ten 10 people become pain-free with normal function after a few months. We have reviewed over 260 people who have had repairs. Of these, 90% had good or excellent outcomes, 8% moderate, and only 2% had a poor outcome. The repaired rotator cuff is twice as strong after surgery compared to before. The age of the person and the size of the cuff tear made no difference to the final outcome.

