INSTABILITY : means that the shoulder dislocates completely (dislocation) or partially (subluxation).
ANATOMY : The shoulder consists of a ball (humeral head) and socket (glenoid). The ball is stabilized in the socket by a cartilage rim (“labrum”, which means “lip”) and the ligaments, which attach to the labrum. In other words these ligaments attach to the socket on the one side and to the ball on the other side
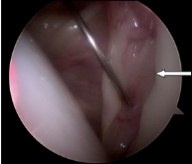
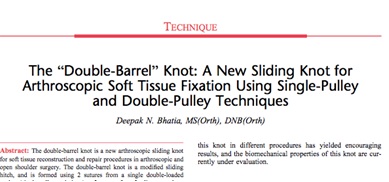
Torn labrum
DISLOCATION : Usually the ball dislocates to the front (anterior). For this to happen the arm is forced upwards, backwards and outwards (abduction and external rotation).
THERE ARE MAINLY TWO TYPES OF DISLOCATIONS :
1. Dislocations due to trauma (injury): During the first dislocation the labrum and ligaments are pulled off the edge of the socket (this is called a “Bankart” lesion). As the head slips over the edge of the socket, the latter knocks a hole into the head (“Hill-Sachs” lesion).
In a number of cases, especially in contact sports like rugby, a piece of bone is also pulled off the glenoid (socket) as well.
2. Dislocations due to lax ligaments: These dislocations may first appear at a relatively young age (16-20 years ) and are a bit more common in girls. They may also have other problems due to the loose ligaments e.g. unstable knee caps, etc. The first dislocation may occur due to minimal trauma in contrast to the traumatic type.
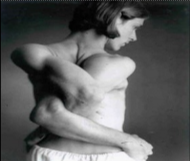
Voluntary dislocater: hyperlaxity of ligaments
With dislocations the patient may be able to reduce the shoulder himself or in many instances may require a doctor or other trained person to reduce it. At times the patient may need an anaesthetic to reduce the shoulder as the muscle spasm may prevent reduction.
SUBLUXATION : This term is used for “partial dislocation” where the shoulder slips out of the joint partially and slips back into position again.
DIAGNOSIS OF INSTABILITY :
1. Clinical: Symptoms of instability :
A dislocation is usually extremely painful and disabling. There is total inability to move the shoulder at this stage.
After reducing the dislocation, pain is significantly reduced and the shoulder is mobile again.
Minor or “subtle” instability of the shoulder is experienced as a feeling of slipping or only pain with certain movements
The deformity of the shoulder is apparent by looking at it from the outside: the upper corner of the shoulder appears “squared off”, a bulge may be felt in front and a hollow at the back.
2. Radiological :
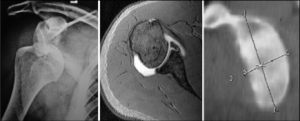
X-Ray : The dislocation may usually be seen very well on an X-ray. These are also relevant to verify that the shoulder is reduced after reduction maneuver.
MAGNETIC RESONANCE IMAGING (MRI) :
MRI is not needed in every case. These scans may demonstrate the presence of a Bankart lesion as well as the rare HAGL lesion (Humeral Avulsion of the Gleno-humeral Ligaments) which is also referred to as a “reverse Bankart” lesion due to the fact that the ligaments tear off the humeral head and not off the edge of the glenoid as is usually the case.
COMPUTER TOMOGRAPHY (CT) SCAN :
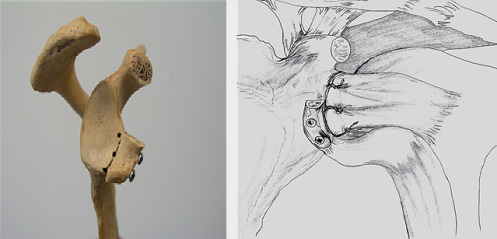
These are done to judge the degree of bone loss on the glenoid edge and also the size of the defect on the humeral head (Hill-Sachs lesion). The size of bone loss of the socket (glenoid) is best seen on a “sagittal reconstruction” view and the Hill-Sachs on the “axillary” view
If significant bone loss is seen on these views a ligament or soft tissue procedure is less likely to be successful and the patient may require a bony procedure, e.g. Latarjet operation to deal with the bone loss.
OUTCOME : A Bankart lesion (ligament and labrum tear) seldom heals and the shoulder dislocates repeatedly whenever the arm is forced upwards and outwards after the first dislocation.
The younger the patient is at the time of the first dislocation, the more likely will he suffer recurrent dislocations (repeated episodes of the shoulder dislocation).
The reason is that in the young, the ligaments are so strong and elastic that they are stripped off the bone with the labrum, rather than tearing, and do not heal back to bone. The rate of recurrence in the under 25-year-old age group is 90-100%.
As the shoulder dislocates repeatedly, progressively more damage is done, the bony lesions become larger, the ligaments stretch out and dislocations occur with greater ease.
Dislocations in older patients result in tearing of the ligaments, which may heal without any problem – the rate of recurrence is much less in older individuals. In older individuals the associated injuries with dislocations are more common: these include rotator cuff tears, fractures, nerve injury and even vascular injury
Dislocation due to ligament laxity causes less damage to the shoulder (it dislocates more easily the first time) and can be managed non-operatively (with rehabilitation) for longer than the post-traumatic type.
TREATMENT : A patient with a Bankart lesion usually needs an operation to repair the ligaments to the bone, even after the first dislocation, as the lesion usually does not heal. As mentioned above, the instabilities due to lax ligaments can at first be managed with exercise and strengthening and only need operations when the symptoms become unbearable.
Does this mean that every patient with instability needs an operation ?
The answer is no. If the person is willing to live with it knowing that he/she has to avoid the position of the arm where it slips out, and does not participate in any strenuous activities which may precipitate a dislocation, they could live with the potential instability for as long as they choose to.
On the other hand, repeated dislocations should be avoided as the joint is gradually damaged more and more. Also consider the fact that certain dangerous activities e.g. sports in deep water or mountain climbing could be fatal if the shoulder dislocated under such circumstances.
VARIOUS OPERATIONS ARE AVAILABLE TO STABILIZE AN UNSTABLE SHOULDER :
Arthroscopic Bankart procedure : It is done with an arthroscope (“key-hole surgery”), although this repair can also be done with an open technique. In our unit we prefer the arthroscopic procedure.
Arthroscopic procedure : Usually three holes measuring about 3-5 mm are made. The arthroscope and the instruments are passed through these holes (referred to as “portals”) The arthroscope relays a picture to a television monitor and the surgeon watches his actions on the monitor. (Refer to the section on Treatments-Shoulder surgery).
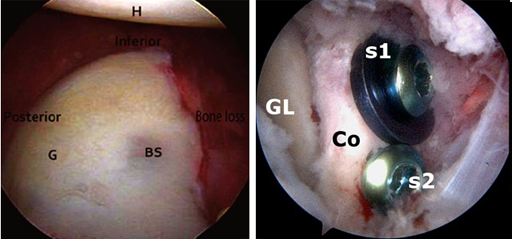
First a roughened area is made on the surface of the bone of the glenoid (socket) to allow the ligaments to heal to this area of the bone. Tiny absorbable devices (“bone anchors”), with sutures attached are drilled into the bone and the sutures used to fix the ligaments to the bone of the socket. Advance techniques are used to make knots outside the joint and then passing them down the small cannulas to the inside of the joint to tie the ligaments to the bone.


Arthroscopic capsular shift : In some cases the shoulder dislocates due to the ligaments being too lax and not due to tearing (Bankart lesion). This is more common in young females.
Strengthening of the surrounding muscles may improve it, but should this fail an operation may become necessary
For the cases of ligamentous laxity with instability the ligaments are tightened using the arthroscopic technique, very similar to the Bankart procedure but with more emphasis on tightening and reducing the laxity of the ligaments.
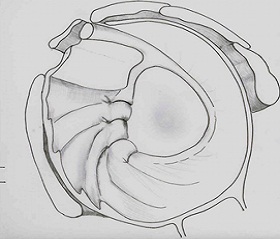
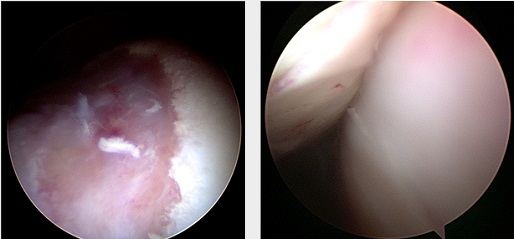
Shifting the capsule to tighten the ligaments (left).
A special knot (right) devised by Dr Deepak Bhatia (named Double-Barrel Knot) is used to secure the shifted capsule in the new position till it heals.
Arthroscopic Remplissage : Remplissage means “to fill in”. This procedure is performed when the bone loss on the ball (humeral head) is moderate to large. The adjacent muscles are attached into the defect with anchors and this prevents failure of the arthroscopic Bankart repair.
The Latarjet procedure (for bony lesions) : If there is bone loss from the edge of the socket, or a large Hill-Sachs lesion (groove in the head of the humerus) the problem becomes more mechanical – referred to as an “engaging lesion” and will not be adequately treated by simply repairing the ligaments as in the Bankart procedure. The Latarjet procedure needs to be done- simply repairing the ligaments will not suffice. The coracoid, a bony outgrowth next to the joint is released and screwed on to the bony defect to fill it. The sling effect of the transferred tendon which is attached to the coracoid also plays a major role in achieving stability This is a highly successful procedure for those few cases that need it. This operation often becomes indicated in contact sportspersons (who frequently suffer bony lesions with their dislocations during the trauma they sustain during their high impact activities) and they will usually be able to return to their previous sport at the same level following this procedure.
THIS PROCEDURE CAN BE PERFORMED OPEN or ARTHROSCOPIC
The arthroscopic procedure is the ALCS procedure described recently by Dr Deepak Bhatia.This procedure involves 6-7 tiny cuts (portals) in the skin and the bone grafting (Latarjet) is performed endoscopically. Simultaneously, the ligaments are also repaired back (Capsular shift).
It is important to note that one of the most common reasons for the Bankart procedure to fail and the patient remaining with instability is the bony lesion not recognized and addressed by the surgeon. In such a case of failed surgery the Latarjet procedure will often rectify the problem.
After the operation : You may leave the hospital on the same or next day. Pain is usually minimal to moderate. The arm will be in a sling, simply to remind you not to move the arm upwards, backwards or outward.
Wear the sling at night while sleeping and when going out. At home it may be taken off, but remember the following restrictions:
While facing forwards and moving the arm, the hand should be visible. As soon as you move the hand backwards, out of sight, the shoulder is in a “danger zone”, and the repair can be damaged.
These precautions must be followed for 3weeks, after which you will receive further instructions.
The shoulder is usually stiff for a few weeks following the operation but this is common and should not raise any concern.
After 3weeks : With guidance, progressive mobilization and strengthening will now be allowed. Weight training, swimming (breast stroke), etc. will be gradually introduced from 6 weeks onwards.
Return to sport : Can be allowed soon after this 6-week period, but for contact sports like rugby, and throwing sports like baseball, 3 months and more of rehab may be required.
It is important to avoid injury during the recovery period to prevent pulling out of the screws
Success Rate : The procedures mentioned above are usually successful to stabilize the shoulder and result in the patient regaining normal function, provided that the operation is tailored to the specific type of instability and is performed with the necessary expertise.
READ DR.DEEPAK BHATIA’S SCIENTIFIC PUBLICATIONS ON THIS TOPIC :
1. Bhatia DN. Arthroscopic Latarjet and Capsular shift procedure. ( under review)
2. Bhatia DN, De Beer JF. Management of anterior shoulder instability without bone loss: Arthroscopic and mini-open techniques. Shoulder & Elbow 2011;3:1-7.
3. Bhatia DN, DasGupta B. Surgical treatment of significant glenoid bone defects and associated humeral avulsions of glenohumeral ligament (HAGL) lesions in anterior shoulder instability. Knee Surg Sports Traumatol Arthrosc. 2013 Jul;21(7):1603-9
4. DeBeer JF and Bhatia DN. Shoulder instability in the middle aged and elderly patients: Pathology and surgical implications. International Journal of Shoulder Surgery, 2010;4.
5. Page RS, Bhatia DN. 2010. Arthroscopic repair of a chondrolabral lesion associated with anterior shoulder dislocation. Knee Surgery Sports Traumatology Arthroscopy. 2010 Dec;18(12):1748-51
6. Bhatia DN. 2012. Arthroscopic “Cuff sparing” percutaneous (CUSP) Technique for posterior instability repair in the beach-chair position. Tech Hand Up Extrem Surg. 2012 Sep;16(3):173-9
7. Bhatia DN. 2012. Dual-window subscapularis-sparing approach: A new surgical modification of the Latarjet procedure. Tech Hand Up Extrem Surg. 2012 Mar;16(1):30-6
8. DeBeer JF and Bhatia DN. 2009. Shoulder injuries in Rugby players. Int J Shoulder Surg, 2009; 3:1-2.
9. Bhatia DN, De Beer JF, van Rooyen KS. 2009. The Subscapularis – sparing approach: A new mini-open technique for repair of the HAGL lesion. Arthroscopy 2009;25(6): 686-690
10. Page RS, Bhatia DN. 2009. Arthroscopic HAGL repair: Anterior and posterior techniques. Techniques in Hand and Upper Extremity Surgery 2009;13(2), 98-103
11. Bhatia DN, deBeer JF, vanRooyen KS, duToit DF. 2007. The “Reverse Terrible Triad” of the shoulder: Circumferential glenohumeral musculo-ligamentous disruption and neurological injury associated with posterior shoulder dislocation. Journal of Shoulder and Elbow Surgery. 2007; 16(3): e13-17.
12. DN Bhatia, JF DeBeer. 2012. The Cape Town Approach for Latarjet Procedure: Is There a Benefit to Flip the Bone Block? In: Shoulder Concepts 2012 Ed. P Boileau. Sauramps Medical Publisher. Pg 71-74
13. DN Bhatia, JF DeBeer, DF Dutoit. 2008. Coracoid process anatomy: Implications in Latarjet procedure. In: Shoulder Concepts 2008, Arthroscopy and Arthroplasty. Ed. P Boileau. Sauramps Medical Publisher. Pg 63-78.
14. DeBeer JF and Bhatia DN. 2009. Shoulder injuries in Rugby players. Int J Shoulder Surg, 2009; 3:1-2.

